01/09/2017
On December 19, the Food and Drug Administration (FDA) granted accelerated approval for rucaparib (Rubraca™) to treat some women with advanced ovarian cancer. The drug is approved for women whose cancers have progressed despite treatment with two or more chemotherapies and whose tumors have a mutation in the BRCA1 or BRCA2 genes, as identified by an FDA-approved companion diagnostic test. About 15% to 20% of ovarian cancers harbor a BRCA mutation.

FDA Approves Rucaparib for BRCA-Positive Ovarian Cancer
January 9, 2017, by NCI Staff
On December 19, the Food and Drug Administration (FDA) granted accelerated approval for rucaparib (Rubraca™) to treat some women with advanced ovarian cancer.
The drug is approved for women whose cancers have progressed despite treatment with two or more chemotherapies and whose tumors have a mutation in the BRCA1 or BRCA2 genes, as identified by an FDA-approved companion diagnostic test. About 15% to 20% of ovarian cancers harbor a BRCAmutation.
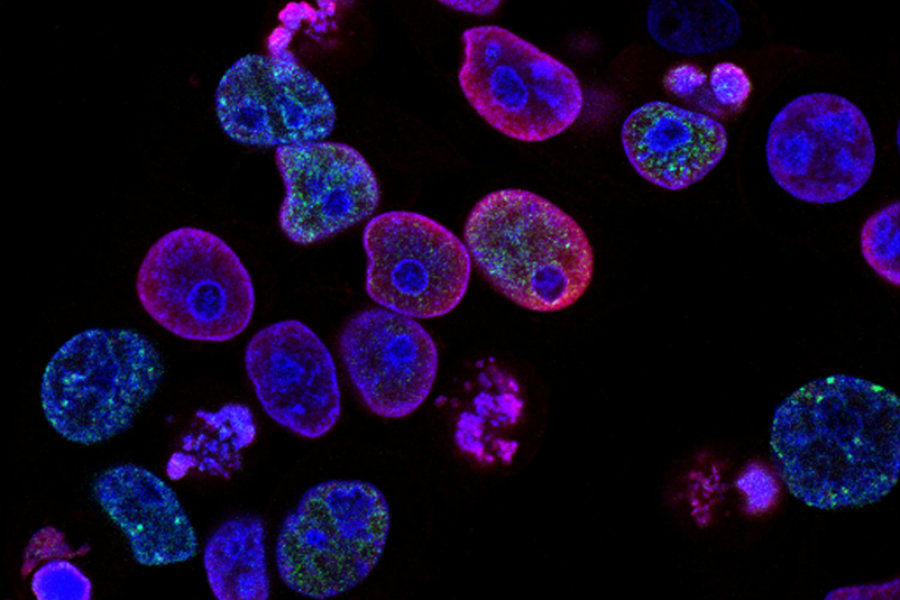
Blocking Cancer Cell Repair Mechanisms
Rucaparib is a type of drug called a PARP inhibitor. PARP inhibitors block an enzyme that normally helps cells repair damaged DNA. When a cell accumulates enough DNA damage, it dies. Cancer cells with BRCA mutations already have defective DNA repair mechanisms, which, studies have shown, make them especially sensitive to PARP inhibitors.
In the two early-phase trials that led to the accelerated approval, a total of 106 women with BRCA-mutated advanced ovarian cancer received rucaparib. More than half had complete or partial shrinkage of their tumors during treatment. These treatment responses lasted a median of just over 9 months. Additional clinical trials testing rucaparib in ovarian cancers with and without BRCA mutations are ongoing.
Common side effects seen in the women who received rucaparib included nausea, fatigue, vomiting, anemia, abdominal pain, unusual taste sensations, constipation, decreased appetite, diarrhea, low levels of platelets in the blood, and trouble breathing. Rucaparib—like other PARP inhibitors—also carries the risk of serious bone marrow problems, such as myelodysplastic syndrome and acute myeloid leukemia.
Rucaparib is the second PARP inhibitor to be approved for BRCA-mutated ovarian cancer. The first, olaparib (Lynparza®), received approval in 2014 for ovarian tumors that have been treated with three or more chemotherapies. A third PARP inhibitor, niraparib, has shown promising results in some types of ovarian cancer, regardless of whether the tumors have BRCA alterations. Niraparib is under review by the FDA for potential approval.
Although PARP inhibitors are currently approved for a relatively small percentage of patients with advanced ovarian cancer, the drugs offer those women an important treatment option, said Ursula Matulonis, M.D., director of the Medical Gynecologic Oncology Program at Dana-Farber Cancer Institute in Boston.
Testing for BRCA Mutations
The companion diagnostic test for rucaparib, the FoundationFocus CDxBRCA test, is the first companion diagnostic test approved by the FDA that is based on next-generation sequencing technology. Next-generation sequencing allows a tumor’s DNA to be rapidly sequenced in full.
Currently, explained Dr. Matulonis, the standard of care for ovarian cancer includes testing newly diagnosed women for inherited, or germline, BRCA mutations, which account for about 80% of ovarian tumors with a BRCA mutation. Testing for germline BRCAmutations does not require next-generation sequencing technology.
Germline testing is done for several reasons, said Dr. Matulonis. It determines whether patients may be candidates for a PARP inhibitor. And it can also provide information to help a patient’s family members decide whether they want to undergo BRCA mutation testing as well.
Tests that use next-generation sequencing can find the rarer cases of BRCA-mutant ovarian tumors caused by somatic mutation—noninherited mutations that arise over the course of a person’s life, explained Dr. Matulonis.
However, because of the very high cost of next-generation testing—and the fact that women often end up paying for such testing themselves because insurance companies are reluctant to—Dr. Matulonis said she doesn’t expect next-generation sequencing to be offered immediately as part of standard care to all women newly diagnosed with ovarian cancer.
But if a woman without a germline BRCA mutation specifically asked for the next-generation sequencing test to see if she could still be a candidate for PARP inhibitor treatment, “I would consider it,” said Dr. Matulonis. “In the future, somatic BRCA testing may not be necessary if the indication for PARP inhibitors is expanded to all women with high-grade serous ovarian cancer,” she added.
Additional research is needed to answer many outstanding questions about the use of PARP inhibitors in women with ovarian cancer, continued Dr. Matulonis, such as whether switching to a different PARP inhibitor once a tumor progresses would provide any benefit.
She and other researchers are also doing clinical trials of PARP inhibitors in combination with targeted therapies, such as angiogenesis inhibitors and drugs that target heat-shock proteins, “to see if we can expand their use beyond cancers with definitive DNA [repair] defects,” she concluded.


































No hay comentarios:
Publicar un comentario